Just like all medical imaging methods, ultrasound has its plus and minuses, helping to exclude or confirm a certain diagnosis. Even though its role is limited to the diagnosis of digestive tract conditions, over the past years, due to the improvement of the US devices (new software, with real-time 3D-4D or sonoCT techniques) spectacular digestive tract images have also been obtained.
The importance of transabdominal digestive tract US is often underrated in clinics. This is due to the sonographic presentation of the digestive tract segments from an anatomic point of view (e.g., the back wall is hard to view because of the gas bubbles inside it). There are certain diseases where US plays a key role: intestinal obstruction, appendicitis, diverticulitis, Crohn’s disease. However, this very much depends on the experience of the operator, the imaging specialist. Moreover, it also helps obtain a real-time diagnosis, with minimum traumas or secondary effects for the patient, especially if the patient is a child or a pregnant woman.
Except for emergencies, a certain training is requested for ultrasound, required in order to obtain a suitable sonic window, with the avoidance of the artefacts generated by the presence of gas, food residues or the increase of the digestive tract lumen discharge (e.g., the presence of the fluid inside the intestine may be a sign of obstruction, inflammatory disease or malabsorption).
The ultrasound examination is performed after a period of rest of approx. 4-6 hours. This does not apply in the case of patients suffering from diabetes mellitus. In this case, a light breakfast is allowed! The examination is performed using a 3-5Mhz frequency probe. 5-10Mhz probes can be used in children or low weight patients, especially if there is a prior diagnosis.
Anatomically, the digestive tract has 5 layers. The thickness of the wall varies: from 5mm (gastric antrum – horizontal section of the stomach) to 1-2mm (duodenum and small intestine). At the level of the colon, the thickness is of approx. 3mm, and in case the colon is filled with air and distended, its size importantly decreases. The width of the digestive tract lumen varies a lot – in the small intestine it is of less than 2cm.
One of the benefits of US is that it allows for the real-time investigation of the peristalsis (digestive tract movements). For instance, in intestinal obstruction, it is akinetic or the loops display hyperperistalsis, which is frequent in intestinal infections.
US Diagnosis of Certain Digestive Tract Conditions:
Acute Appendicitis: The appendix is located retrocecal (the first section of the ascending colon) and it has the appearance of a closed-end tubular, round/ovalar structure, without peristalsis and often with intraluminal air. It has an anteroposterior diameter of approx. 6mm. It is compressible with an echogenicity similar to that of the small intestine. In the case of appendicitis, its diameter increases, it loses its compressibility, displays pronounced vascularization and, very importantly, it is painful upon examination and transducer pressure.
Colon Diverticulosis: It is characterized by colon abnormalities, displayed as mucous and sub-mucous membrane “POCKETS”, which cross the wall and protrude outside its contour. The incidence is of 50% in adults and it is often located at the level of the sigmoid and of the descending colon. US has a sensitivity of 84% and a specificity of 85% in their diagnosis, if 2-4 Mhz transducers and abdominal compression are used. It has a round / ovalar structure, with increased echogenicity and posterior attenuation, with a mixed air/gas/faeces content.
Colon Cancer: It generally occurs men above the age of 40-50. Heredity plays an important role, alongside an insufficient fibre intake. Such patients may feature colon polyps, family colon polyposis or inflammatory bowel diseases. The US diagnosis is casual and it is only possible in sizes above 2cm. Our attention is drawn by the irregular thickening of the colon wall, the absence of the normal peristalsis and of the anatomic colon wall layers, and a tumour mass is identified on the posterior abdominal wall upon palpation. The main role of the ultrasound is to allow for the precise viewing of the intrahepatic metastases, which largely depends upon the examiner’s experience, the performance of the device and, last but not least, on their size. In most cases, they display as hyperechoic lesions (as compared to the hepatic echogenicity), some with a hyperechogenic halo, but they can also be hyperechoic with a glowing centre – the appearance of a multicentric target, relatively uniformly distributed in both hepatic lobes. Sonography can also provide the following information with regards to colon masses: the affected segment, the infiltration of the neighbouring structures and organs, locoregional lymphadenopathy, the degree of stenosis and the intestinal obstruction risk.
Inflammatory Colon Diseases: Of these, we can mention: Crohn’s disease or ulcero hemorrhagic colitis. These are diseases that affect the large segments of the colon or of the small intestine, with changes in the wall thickness, without full penetration of the same, with the disappearance of the peristalsis and pericolic thickness changes (Crohn’s disease fibrosis changes). Ultrasound is also used to monitor the evolution of the disease. Infectious colitis, specific to the descending colon, are diagnosed by US – thickening of the mucous and sub-mucous membrane (which become hypoechogenic), with normal pericolic fat. A reduced intraperitoneal liquid collection and small locoregional adenopathies can also be noted.
Inflammatory Stomach Diseases: (gastritis, ulcer) are not usually visible upon US, being diagnosed through endoscopy or contrast material (barium) stomach examination. Perforated ulcer is easy to diagnose, through the display of the intraperitoneal air, located around the liver. US plays a limited role in tumour diagnosis. Scirrhous gastric carcinoma (linitis plastica) is very easy to diagnose by US, due to the accentuated thickening of the wall (more than 10mm) with the loss of the normal stratification, changes that are not viewable through other imaging methods (as mentioned above). The gastric wall is rigid in real-time!
Gastric antrum masses area easily viewable after the prior administration of water to the patient.
Intestinal Obstruction: US is useful in emergency situations: a proper viewing window (no pneumoperitoneum or exaggerated intestinal gas content), an intestinal obstruction diagnosis may be set, actually specifying its type (MECHANIC, DYNAMIC) and its age.
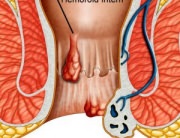
Rectum: It is very difficult to examine, the specific procedure applied depending upon the anatomic segment: the rectal ampulla can be screened transabdominally, the rest of the segment being examined through transperineal or transrectal screening (in women, it is also visible upon transvaginal screening). It also has 5 layers, 4mm thick. Rectal masses represent approx. 58% of the large intestine malignant tumours. Sonography allows us to appreciate the location of the mass, its penetration into the thickness of the walls and neighboring organs, as well as its vertical extension and its ratio to the anal sphincter. In addition, this examination also allows us to appreciate the perirectal adenopathies.
CONCLUSIONS: Ultrasound screening is very useful in diagnosing digestive tract conditions (tumours, inflammatory diseases, neoplasm staging, the display of the regional and remote adenopathies, metastases), in the diagnosis of acute disorders in children, as well as of emergency conditions.