Osteoporosis is a disease most common at women that causes the fragility of the bones and a predisposition to fractures. This is a condition with severe consequences on health and the quality of life. Some women – especially those who do not have access to medical care – experience fractures that could be prevented if osteoporosis is timely treated. On the other hand, not all women who suffer from bone thinning must worry.
Osteoporosis medication producers have developed advertising campaigns addressing women and medical service providers, causing many women to panic and use medication uselessly, ignoring the severe risks and secondary effects.
Over the past years, a number of osteoporosis drugs were launched, which also led to a dilemma amongst the female population as to the right medication for them. More specifically, women want to know when it is advisable to use osteoporosis medication and what are the safest and most efficient treatments. The National Women’s Health Organization believes that the efforts to promote the health of the bones must focus on the prevention of fractures instead of bone mass loss prevention, especially amongst women with a low fracture risk. As it shall be illustrated below, medication is not always the most efficient approach.
This information is meant to help women understand a few aspects related to osteoporosis – what it is, the screening tests, the treatment and prevention using prescription-based medication, alternative prevention approaches. This information can help women make informed decisions on the osteoporosis medication suitable for them or as to whether they should use such medication or not.
What Is Osteoporosis?
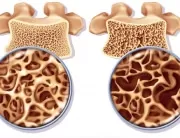
Literally, osteoporosis means porous bone. Throughout our lives, bones constantly go through structural changes. A natural process, which deploys at a microscopic level, destroys and reconstructs the bone tissue. Pregnant women decompose bone tissue to transfer the necessary minerals to the developing fetus, and the bone resistance is restored after childbirth. After the age of 35-40 everyone loses bone mass, because the resorption process is more accelerated than the bone formation process. Around the menopausal age, women lose bone mass at an accelerated rate, probably because of the fact that they no longer need the additional mineral deposits for the development of the fetus.
Osteoporosis is often encountered in the elderly, when bones become fragile and weak. Osteoporosis has several causes – age may be a factor as such, especially in people whose bones did not develop at maximum capacity during infancy and youth. Some type of medication can cause osteoporosis – e.g., the high steroid doses administered for a few months can cause massive bone loss. The surgical ablation of ovaries increases the risk of osteoporosis. A sedentary lifestyle is another cause – astronauts and people with locomotion disorders can develop bone fragility.
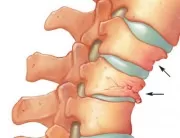
People suffering from osteoporosis are prone to bone fractures, especially in the hip, vertebrae and wrists. Hip fractures require hospitalization, they heal slowly, and many women never fully recover. A vertebral fracture can be unpainful and without any symptoms, but multiple fractures can be very painful and they significantly limit the displacement capacity.
Osteoporosis Screening:
30 years ago, women health supporters were concerned that the effects of bone fractures on elderly women’s quality of life were omitted by the medical community. A change was required – but this change was too radical. Over the past 10 years, large medical companies resorted to promotion campaigns to convince women and medical service providers that osteoporosis does not only affect elderly women, but also middle-aged women. Even though independent medical experts do not recommend osteoporosis tests in women below the age of 65 – except for those exposed to an unusual risk factor, such as the long-term steroid administration – the osteoporosis screening tests are promoted by physicians and medical companies even amongst women aged 40-50.
The most widespread screening method is DEXA scan, which measures the mineral density in the hip or the spine. DEXA scan results compare women’s bone density to the bone density of a healthy young adult (almost guaranteeing a result that shows bone mass loss, considering that a person does lose bone mass in time). If women’s bone density is significantly lower than the one used as reference, they are diagnosed with osteoporosis. Some clinicians classify bone densities that are a little below the normal bone density as “osteopenia” – a term describing a low bone density, but which is not a disease or a medical condition.
DEXA devices are safe and they do not pose any risks for the health, but their timely use to diagnose osteopenia can lead to the commencement of a useless treatment. As a result, women use for tens of years expensive medication with potentially severe secondary effects. Moreover, even though scanning can predict the short-term fracture risk, it is unable to accurately predict the risk of fractures over a longer period of time; thus, a test performed at the age of 45 is unable to predict the risk of fractures at the age of 70 (when most women suffer debilitating fractures).
Moreover, there are big differences between the devices developed by the same manufacturer. These differences can lead to an error that is as high as any density change that the tested person incurs. Hence, it is recommended that the tests are resumed at least once every two years and, preferably, on the same device.
There also are unanswered questions regarding the value of these tests for women of color. The initial DEXA studies did not include any women of color, so there is a major information gap regarding the normal bone density values that could pose a risk for this population. In general, African American women have denser bones and a lower risk of fractures than Caucasian women; American-Asian women have thinner bones, but also a lower risk of fractures than Caucasian women. The National Women’s Health Organization believes that the cases of osteoporosis should be investigated in all ethnicities and that DEXA scans are required amongst women of color; until these investigations are performed, caution is recommended in the performance of tests and the interpretation of results.
The osteoporosis diagnosis in young women generally involves several stages. Even though these stages may be different depending on each case, they include:
- the medical history;
- the physical examination;
- osteodensitomety (bone density measurement);
- laboratory tests;
- X-ray scans.
Medical History. The medical service provider may request information on the medical history. Here are some of the questions you should expect:
- Did you experience bone fractures as an adult?
- Did one of your parents suffer from osteoporosis? Did your parents experience bone fractures as adults?
- Have you, your parents or siblings ever suffered from kidney stones?
- Is your menstruation regular?
- Do you have digestion and intestinal transit problems?
- Do you use medication? Did you take medication in the past?
- Have you ever been diagnosed with a medical condition or health problems?
- Do you eat calcium-rich foods, such as milk, yoghurt or cheese? Do you take food supplements?
- How often do you exercise and what kind of exercise do you engage in?
- Have you ever smoked?
- Do you drink alcohol?
Physical examination. The medical service provider may assess certain risk factors or osteoporosis signs through:
- height and weight measurements;
- the calculation of the body mass index;
- spine examination.
Bone Density Measurement. The bone density is measured using a special device for postmenopausal women and men above 50. This test measures the bone density of the hip, spine or other bones and it is the optimum osteoporosis diagnosis method in the elderly. This test should be performed using a DXA device (Dual-energy X-ray absorptiometry).
The osteoporosis diagnosis in postmenopausal women is not direct and may be quite complex. Firstly, the bone density tests are not recommended for young women.
Here are some reasons:
- Most postmenopausal women with a low bone density do not face a high risk of fractures in the near feature. Hence, the detailed bone density information can be a cause of useless concern.
- Some postmenopausal women may have a low bone density because they genetically have a low bone mass limit. Nothing can change this genetic aspect.
- DXA scans can generate lower bone density values for short and slender women. Thus, the DXA test can indicate a low bone density value in a short person, but the bone density is normal when correlated to the body dimensions.
- Osteoporosis medication is not recommended to postmenopausal women. Bone densitometry tests are used to help make treatment-related decisions.
Osteodensitometry tests are performed in these women if their bones fracture easily or if they suffer a hip or spine fracture, which is unusual for their age. Moreover, if you suffer from another medical condition or take a drug that has osteoporosis as a secondary effect, an osteodensitometry test may be required. The medical service provide may recommend this test if they are concerned about the health of your bones for other reasons.
Interpretation of osteodensitometry results. Osteodensitometry results display two values: the Z and the T score. If the medical service provider recommends this test, the Z score and other information shall be read in order to decide whether you suffer from osteoporosis or from another bone condition. The Z score compares the bone density to the normal one for a person your age. Even though the Z score is not used as such to diagnose osteoporosis in postmenopausal women, it can offer important information.
Here is some information to understand the Z score:
- According to the International Society for Clinical Densitometry, if the Z score is above 2, the bone density is regarded as being within normal limits for your age. For instance, a score of +0.5, -0.5 and -1.5 is regarded as normal for most postmenopausal women.
- If the Z score is 2 or less, the bone density is regarded as being below the normal limits (e.g., -2.1, -2.3 or -2.5). If the Z score falls within these values, the physician will assess your medical history and the possible bone mass loss causes, including secondary osteoporosis, before setting the osteoporosis diagnosis.
- If the Z score is normal, but you did suffer one or several fractures following minor injuries, the physicians can set an osteoporosis diagnosis, because people with a normal bone density very easily suffer from fractures.
As mentioned above, the bone densitometry test will also display a T score. This score compares the bone density to the normal one for an adult aged 30. T scores are used to diagnose osteoporosis in postmenopausal women and in men aged above 50, but not in premenopausal women.
Resuming the bone densitometry test. The test is resumed after 1 or 2 years to determine if a person has a low maximum bone mass limit or whether that person loses bone mass. If the bone density decreases a lot in-between the two tests, this is an indication of the fact that the person is losing bone mass and the tests need to be continued.
Required laboratory tests. If you have low bone density or osteoporosis, your physician may perform certain tests to find out what is happening in your body.
These tests, which are not recommended to anyone, will determine:
- if you have a sufficient vitamin D level;
- if you suffer from a condition that causes bone mass loss;
- if you lose bone mass faster than normal.
X-ray scans are the most frequently used method to diagnose fractures. Sometimes, vertebral fractures are unpainful. The physician may recommend a vertebral X-ray especially if:
- you fell from a height;
- you have a bent or squat body posture;
- you experience back pain.
Medication osteoporosis treatment in women:
Women diagnosed with osteoporosis or osteopenia are recommended prescription-based medication, to prevent the subsequent bone mass loss and mitigate the fracture risk. The most frequently used drugs are:
Hormones: The Food and Drug Administration has approved the Estrogen and Progestin treatment to prevent osteoporosis, but not to treat it. Both estrogen and estrogen and progestin combinations reduce the risk of osteoporosis and fractures in women. However, hormones also increase the risk of mammary cancer, heart attacks, strokes and pulmonary embolisms. That is why hormones are the last resort solution to prevent osteoporosis, being recommended only if other prevention methods fail or are not advisable in certain particular cases.
Other two hormones were approved as osteoporosis treatment: Teriparatide and Calcitonin. Teriparatide (Forteo) is a derivative of the human parathyroid hormone (parathormone), the main bone calcium and phosphorus regulator; it has been shown that a daily injection of 20 mg stimulates the formation of new tissue and prevents vertebral, hip, wrist or other bone fractures in women suffering from osteoporosis. Teriparatide is generally used only in women suffering from severe osteoporosis, because most people do not enjoy daily injections, and the secondary effects include nausea, muscle cramps in the legs and a dangerously high calcium level. It also is very expensive, and some insurance companies are reticent when it comes to covering the costs.
Calcitonin (Fortical or Miacalcic – not to be mistaken for calcium supplements) have demonstrated their efficacy in preventing vertebral fractures, but not hip or wrist fractures. It was approved for the treatment of women suffering from osteoporosis, but the approval relied on weaker results than the ones obtained with more recently launched medication, and, in general, its use is not recommended. Women using calcitonin should monitor the calcium intake in their food, as excessive calcium consumption is dangerous. Calcitonin is administered as a nasal spray; the secondary effects include nasal congestion and nausea.
Bisphosphonates: Currently, a number of 6 bisphosphonates are approved to prevent bone mass loss and fractures in postmenopausal women: Alendronate (Fosamax), Etidronate (Didronel), Ibandronat (Boniva), Risedronate (Actonel), Tiludronate (Skelid) and Zoledronic acid (Reclast, Zometra). Some are daily administered, others are for weekly or monthly use. Bisphosphonates apparently have lower risks than hormones, at least during the first five years of administration. However, the drugs have not been available on the market for a long period of time, so the risk associated to their use for more than 10 years or of their use by premenopausal women could not be assessed. It is a well-known fact that the benefits of at least one bisphosphonate (Alendronate) persist for many years after the treatment is interrupted. It could not be determined whether its administration to middle-aged population has reduced the older age fracture risks.
A few possible medical conditions were associated to bisphosphonates. Firstly, there are unanswered questions with regards to their effect on the heart. The US Food and Drug Administration announced in January 2010 that they were conducting a drug safety research, initiated after some women reported irregular cardiac rhythm rates (atrial fibrillation) higher than in other women. Secondly, women may experience severe bone, joint and muscular pain after they start taking bisphosphonates. The Food and Drug Administration recommends the interruption of the administration in these cases, in order to eliminate pain. Thirdly, it has been shown that the maxillary bones dies in certain women (maxillary necrosis), which may require its removal. Fourthly, recent findings have expressed a concern with regards to the association of bisphosphonate administration and atypical femoral fractures. Finally, bisphosphonates may cause gastric acid burns, ulcer and they can affect the stomach and esophagus if not they are not administered under strict dietary conditions (on an empty stomach, with a glass of water, after you’ve been standing for approximately an hour).
Selective estrogen receptor modulators:
Raloxifene (Evista) has been relatively recently approved to prevent and treat osteoporosis. The drug was more extensively treated than bisphosphonates and, even though it mitigates the risk of vertebral fractures, it seems it does not reduce the hip fracture risk. Moreover, it raises questions with regards to the secondary effects: the risk of blood clots, hot flashes, nausea and leg cramps. In September 2010, another drug was approved, Lasofoxifene, to treat osteoporosis in postmenopausal women. Subsequent researches have shown a reduction in the number of vertebral fractures during the first three years of use. Just like Raloxifene, Lasofoxifene increases the thrombose, as well as the vaginal bleeding risks; women who used this drug were subjected to more invasive procedures, such as endometrial biopsies, dilation and curettage or even hysterectomy. The National Women’s Health Organization has recommended that the approval of Lasofoxifene be postponed until the use over 5 years highlights the effects and efficiency of the long-term use. The Organization has also expressed its concern that Pfizer, the company producing Lasofoxifene, will encourage women to use this drug for health conditions that were not sufficiently evaluated.
Treatment alternatives:
Bone development and strengthening can also be achieved otherwise than by using drugs. The osteoporosis prevention researches were revised and clear scientific proof has been identified that the calcium and vitamin D intake is essential for the development and maintenance of bone health.
Regular physical exercises (especially the resistance ones and high impact activities) contribute to the development of the bone mass. Other promising activities focus on preventing fractures: balance training reduces the risk of falling, which generally is the main cause of bone fractures in the elderly. A few limited studies have shown that hip protectors and the patient’s education on their use may reduce the fracture risk, but more extended studies did not reveal any advantages. Other practical methods to mitigate the risk of falling include: the update of vision drug prescriptions, the verification of the secondary effects of medication inducing dizziness, the elimination of indoor slipping hazards (slippery rugs), suitable footwear.
Conclusions:
Pharmaceutical companies are trying to expand the osteoporosis drug market; their recent efforts concern the non-traditional population testing (young women and men). Many women below the age of 65, without high risk factors, are tested for osteopenia and osteoporosis, despite the fact that preventive testing has not been shown to prevent severe fractures. The International Women’s Health Coalition encourages women below the age of 65 to refuse bone density tests, especially if they do not face unusual circumstances that increase the fracture risk.
Apart from the bone fracture risk assessment, women should also consider the need of osteoporosis drug administration. Moreover, the duration of the treatment is critical in determining the efficiency: the interruption of a preventive treatment causes the quick loss of the preventive effects. Contact your physician for details on the safety and efficiency of osteoporosis drugs or the use of alternatives other than drugs, depending on your medical history and your current health condition.